
What is insulin?
Insulin is a lifesaving medicine for students with type 1 diabetes, and most will need to take it at school.
Insulin is a hormone that regulates glucose levels. It does this by allowing glucose from the bloodstream to enter cells around the body, where it is used for energy. Without insulin, glucose builds up in the bloodstream, which can make a person extremely unwell.
People with type 1 diabetes must give themselves insulin every day for life. Insulin cannot be taken as a tablet. It must be injected, using an insulin pen or syringe, or given via an insulin pump.
Some students will be able to give their own insulin, and some may need support from school staff. Designated school staff must be trained to provide support with giving insulin.
Types of insulin
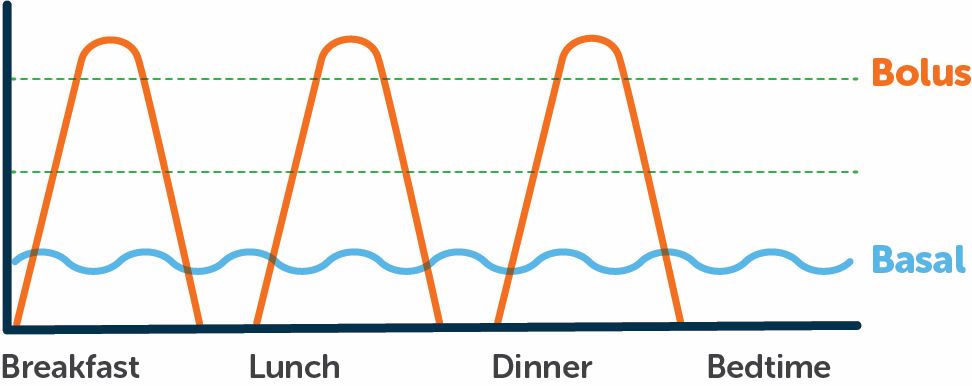
Students with type 1 diabetes may use different types of insulin at different times of the day.
-
Bolus insulin
Bolus insulin is given at mealtimes when a student eats carbohydrates (carbs). Bolus doses use rapid-acting insulin to manage the rise in the glucose level following a meal. Sometimes, a bolus dose may also be given to treat a high glucose level. This is known as a “correction” dose or bolus, as it “corrects” the glucose level by bringing it back into target range.
Bolus doses are calculated based on the amount of carbs the student plans to eat or drink, and/or their blood glucose level.
-
Basal insulin
Basal insulin is also known as background insulin. This type of insulin manages a student’s glucose level overnight and between their meals. Basal insulin may be injected at home using a long-acting insulin or continually infused via an insulin pump.
-
Mixed insulin
Some students may use mixed insulin, which is a combination of bolus and basal insulin. Mixed insulins are less commonly given at school, but they may be given in specific circumstances (e.g. if the student has early morning sport).
Giving insulin
Students with type 1 diabetes will usually need to give an insulin bolus with food, for example at recess and/or lunchtime. It is important that insulin is taken on time before or with food as per the student’s diabetes management plan.
School staff are not expected to make independent clinical decisions about insulin doses. School staff may be expected, with training, to calculate insulin doses using a specific method documented in the student’s diabetes management plan.
The diabetes management plan will also outline their insulin delivery method, preferred injection sites (if relevant), and any staff support or supervision they may need.
-
Injecting insulin with a pen or syringe
Many students will inject their insulin using an insulin pen, or less commonly a syringe. Insulin is absorbed best when injected in the fatty layer just beneath the skin. The preferred site to inject insulin is the abdomen, although it can also be given in the outer thigh or buttock.
-
Using an insulin pump
Some students may use an insulin pump. This is a small, computerised device that delivers small doses of rapid-acting insulin automatically throughout the day and night. Insulin is delivered through a small flexible tube that sits under the skin. Mealtime and correction doses are given by entering information into the pump or a linked device such as a mobile phone.
Students may need support with this task, which will be documented in the diabetes management plan. School staff are not responsible for adjusting, programming, or maintaining the pump. Their role is to confirm the information entered into the pump or linked device, follow the student’s diabetes management plan, and respond to any alarms.
Insulin storage and sharps disposal
It is important to store insulin correctly, so it remains effective.
Opened insulin
Should be kept safely stored at room temperature (below 25°C) for up to 28 days.
Unopened insulin
Should be stored in the fridge (away from the freezer/chiller section) at 2–8°C.
Avoid extremes
Never freeze insulin or expose it to direct sunlight or extreme heat. Any frozen insulin must be thrown away.
Dispose of used sharps in Australian-standard approved plastic containers. Do not use glass or cardboard containers, tins or plastic bottles to dispose of sharps.
Reasonable adjustments
Reasonable adjustments to support students in managing their insulin at school may include:
- ensuring a current diabetes management plan is available
- training designated staff on giving insulin or providing support and supervision
- providing a safe, comfortable, and private area for the student to take their insulin if requested
- actioning any specific advice in the diabetes management plan about the student’s participation in sport, excursions, camps, exams, and other activities
- implementing infection control measures including providing clear instructions to staff on how to prevent infection and cross contamination when checking blood glucose levels and giving insulin.
Last updated: September 2025


